What is Medical Coding and Billing?
By: Jenn Hall | Updated October 2024
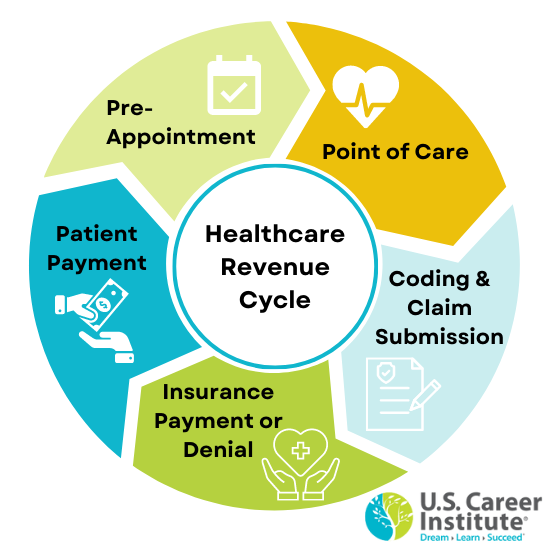
Medical coding and billing are essential functions of the healthcare revenue cycle, ensuring medical providers are reimbursed for services delivered.
Although they are often grouped together, medical coding and medical billing are separate processes, with unique goals and responsibilities.
What is Medical Coding?
Medical coding is the conversion of healthcare procedures, diagnosis, equipment, and medical services into the universal medical alphanumeric code. The information is gathered from physicians’ notes, patient records, lab results, and other documentation and is transformed into code that insurance companies can clearly understand and interpret. There is a medical code for every medical procedure and diagnoses, as well as medical equipment or supplie used to treat the patient.
Every time a patient sees a healthcare provider, medical coding happens. At every visit, the healthcare provider makes an expert assessment based on patient concerns, a medical evaluation, and the patient's medical history. The documentation of the patient visit is added to the patient’s health record. This information helps medical coding professionals identify the relevant medical codes for the services provided and supports the medical billing process.
Medical codes tell payers:
- Diagnosis of the patient
- Medically necessary treatments, services, and supplies the patient received
- Services, treatments, and supplies provided to the patient
- Medical conditions and unusual circumstances that affected the treatment and services
To ensure accuracy, medical coding professionals must stay current on the latest medical coding standards, including ICD-10-PCS, ICD-10-CM, HCPCS, and CPT.
With accurate medical codes documented and associated with each patient interaction, healthcare teams can communicate more effectively with one another. Also, medical billing teams can prepare and follow up on medical claims for reimbursement and avoid unnecessary billing mistakes.
After the medical coding professional has entered the appropriate codes into the system, they are passed on to the medical biller for review and processing.
What is Medical Billing?
Medical billing is the process by which healthcare organizations prepare, submit, and follow up on claims with health insurance companies and/or patients to receive payment for services rendered.
Medical billing professionals review the medical codes associated with the patient visit to identify billable services. They then review the patient’s healthcare insurance information to determine relevant coverage. With this information, they can accurately prepare a billing claim to seek reimbursement.
After the health insurance payer reviews the claim, they will respond with the amount they will pay against the full amount. The final bill will take into consideration existing patient balances, copays, deductibles, and other factors. If the health insurance provider does not cover the procedure or services provided to the patient, or if they only cover a portion of the total cost, the medical biller will invoice the patient for the remaining amount owed. In either case, the medical biller is responsible for following up on billing claims to ensure payment is received and will invoice the patient for the remaining amount owed.
What are the Primary Responsibilities of a Medical Coder and Biller?
Although medical coding and medical billing are closely aligned, they serve different functions within the healthcare revenue cycle. Depending on the healthcare facility, the roles may be combined into one medical coding and billing position, or they may be separated to account for an individual medical coder and medical biller.

Some of the primary responsibilities of a medical coder and biller include:
- Reviewing health information and patient data
- Assigning codes to the diagnoses, treatments, symptoms, and other relative information from the patients visit, using classification software
- Entering charges into a system, report, or form to create a claim
- Ensuring accuracy, completeness, and appropriateness of the data
- Posting payments as they are received
- Sending claims to the appropriate payer
- Following up with payers, such as patients and insurance companies
How Can I Become a Medical Coding and Billing Professional?
At a minimum, you will need to have your high school diploma or equivalent to be considered for an entry-level medical coding and billing position. Some employers will also require candidates to have specialized knowledge of standard medical coding frameworks (e.g., ICD-10, CPT), billing processes, and other healthcare standards (e.g., HIPAA). A great way to develop that knowledge is through an accredited training program and professional certification.
Learn more about medical billing and coding certification from U.S. Career Institute and how you can begin your career as a medical coder and biller in as little as little as 5 months!
