Why Medical Billing and Coding is Important
By: Joann Owens, Nurse turned Medical Writer | August 2023
Medical billing and coding is an important part of the healthcare system. It ensures that care providers bill insurance companies accurately and patients are not left paying more than they should. Medical billing and coding also help in gathering important data regarding the patient's care - their treatments, procedures, and overall experience.
What is Medical Billing
Medical billing is the process of filing and following up on claims with insurance companies to obtain payment for the services rendered by healthcare providers. The whole process is done by professionals called medical billers.
What is Medical Coding
Medical coding, on the other hand, is the process of transforming the patient's data (from diagnosis to treatment plan) to universally accepted alphanumeric codes. These codes are sent to the insurance company (also known as the payer) as part of the process of submitting medical claims.
Medical coding professionals who do this are called medical coders.
How Medical Billers And Coders Work Together
Medical billers work with patients, healthcare providers, and insurance companies. Their main job is to get the appropriate reimbursement for the medical services rendered by the provider or provider organization.
To process claims, medical billers work hand-in-hand with medical coders.
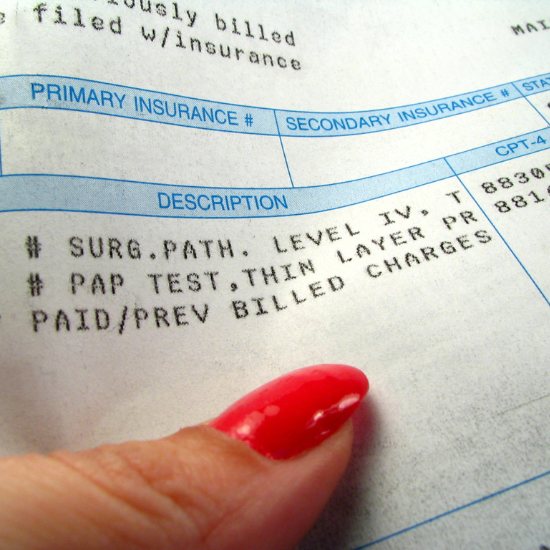
When the patient checks out, the medical report from that visit is sent to the medical coder. The medical coder then translates the information into a report using universally-accepted codes. This report, which also includes the patient’s demographic information, medical history, and all other information pertinent to his care, is referred to as the “superbill.”
The superbill is then passed on to the medical biller (usually through a software program) who then takes this into a billing software or enters it into a paper claim form. This medical claim also includes the total amount they expect from the payer (as stated in the payer’s contract with the patient and provider).
Once the claim is created, the biller is responsible to make sure that the claim meets the standards for compliance. This includes ensuring that the procedure codes are billable, following the patient’s insurance plan and the payer’s regulations.
Billers also make sure that the filing of claims follows the guidelines set by the Health Insurance Portability and Accountability Act (HIPAA) and the Office of the Inspector General (OIG). Unless the claim is for high-volume, big payers like Medicare or Medicaid, billers have to submit their claims through a third-party organization called a clearinghouse. A clearinghouse reformats these claims and makes sure that the right procedural and diagnosis codes are used before submitting them to the payers.
Once the claim reaches the payer, it gets into the process called adjudication. During this process, the payer evaluates the medical claim and decides if this is valid, and determines how much the provider will be paid for.
If the claim is accepted, the payer processes the payment following the agreement it has with the patient/subscriber.
If the claim is rejected, such as in cases of missing patient information or miscoded procedure or diagnosis, it will be returned to the biller. The biller then has to correct the claim and resubmit it for re-evaluation.
Medical billing and coding is an integral part of the healthcare system. These services enable insurance companies to get billed appropriately for the patient's care and healthcare providers to get paid for the services they rendered. Without medical billers and coders, filing medical claims can become a very complicated process. And this can affect everyone in the healthcare system - from patients to healthcare providers and organizations.
If you are interested in playing an important role in the healthcare system then start working towards becoming a Medial Coder, Medical Biller or learn how to do both with an Online Medical Billing and Coding Program.
