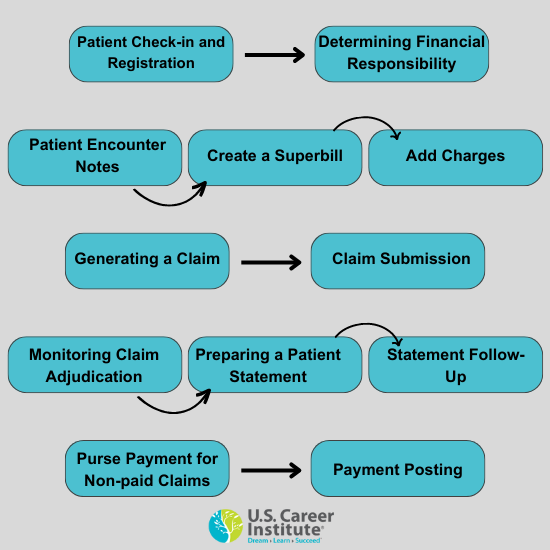
What are the Steps in the Medical Billing Process?
By: Valerie Smith, RN | August 2023
August 2023
Medical billing is an important part of the healthcare revenue process, if you are interested in learning more about what medical billing and coding is, then check out our blog “What is Medical Billing and Coding?” Medical billers are responsible for ensuring that services are correctly billed and paid for. Medical billing specialists will undergo a series of steps to complete the medical billing process for the medical provider to receive reimbursement for patient services.
Patient Check-in and Registration
The patient will complete intake forms, or if a return visit, they will review and update necessary information for the visit and insurance. Gather basic patient demographic information, including their name, date of birth, and the reason(s) for the visit.
Also, the medical billing specialist will identify the patient's identification and collect the patient's insurance information, including the insurer's name and policy number. The medical biller will verify the accuracy and validity of the insurance information by contacting an insurance representative or entering the information into medical billing software. A patient file or medical record will initiate the medical billing process.
Determining Financial Responsibility
The medical billing specialist will determine the financial responsibility for the visit by identifying which medical procedures the insurance will cover. If the patient has secondary insurance, ask them to provide the insurance card and verify their coverage and benefits to identify if the secondary provider will pay the remainder of the bill. The medical billing specialist will notify the patient of any deductibles, co-pays, or balances due for procedures not covered by their insurance.
Patient Encounter Notes
During the patient's visit, each healthcare professional must meticulously note treatments, diagnoses, prescriptions, and services rendered to submit medical claims accurately and receive payment.
Creating a Superbill
After the patient checks out, a medical billing coder will translate the medical report into a diagnosis and procedure code (ICD, CPT, HCPCS, and modifiers) to create a superbill. The superbill will include the patient's demographic information and medical history, procedure and service information, and the appropriate diagnosis and procedure codes.
Add Charges
Medical billing and coding codes standardize medical services. However, the medical billing specialist must add the facility's charges for the claim.
Generating a Claim
The information from the superbill will prepare a medical claim and be submitted to the patient's insurance provider. The medical billing specialist must review the claim to ensure it follows payer and HIPAA compliance standards.
Claim Submission
After reviewing it for accuracy and compliance, the medical billing specialist will submit the claim. The medical billing specialist will often electronically submit the claim to a clearinghouse, a third-party company between healthcare providers and the insurance provider. However, high-volume payers, such as Medicaid, will accept claims from healthcare providers. Some payers have specific guidelines for claims submission that require the medical billing specialist to follow accurately.
Monitoring Claim Adjudication
Payers will evaluate the medical claim and determine whether it is valid and compliant and the provider's reimbursement amount through adjudication. The claim may be accepted, rejected, or denied. The provider will receive payment according to the insurer's agreements with an accepted claim. A rejected claim contains errors and requires correction before resubmission. The payer refuses to reimburse the provider if a claim becomes denied. The medical billing specialist must notify the patient of a denied claim and that they owe the provider the non-reimbursed amount. In contrast, ask the patient if they have secondary insurance.
Preparing a Patient Statement
After processing the claim, the medical billing specialist bills the patient any outstanding charges. The patient will receive a detailed statement explaining the procedures and services, costs, the amount the insurance paid, and the amount the patient owes the provider.
Statement Follow-up
The medical billing specialist ensures the healthcare facility receives payment for all claims or outstanding balances. In addition, the medical billing specialist follows up with patients with a statement to make arrangements to accept payment for delinquent accounts or submit to collection agencies. The statement must include payment due dates and instructions on how the patient can pay their balance.
Pursue Payment for Non-paid Claims
The medical billing specialist must monitor accounts receivable to identify when reimbursement claims are taking longer than expected—follow up with the patient for payment for denied claims.
Payment Posting
The medical billing specialist will post payments to the patient's account and deposit the received payment to the healthcare facility's account.
Medical billing plays a critical role in the healthcare revenue cycle, it can also be an exciting career! If you are interested in learning more about becoming a medical biller, check out our online medical billing program.
