Careers
Careers
March 03, 2025
Career Profile: Dental Assistant
Explore a rewarding career as a Dental Assistant! Learn about job responsibilities, education paths, certification options, salary potential, and industry growth.
Careers
October 31, 2024
Exploring a Career in Medical Coding and Billing
Medical Coders and Billers play an essential roll in the healthcare revenue cycle. Explore the awarding career in medical coding and billing.
Careers
April 21, 2025
What is Health IT
Health IT is an important role in the healthcare system. Learn what Health IT and its role in the healthcare system and how to start a career in the field.
Careers
April 21, 2025
Becoming a Coding & Billing Specialist
Medical coding and billing is an essential part of the healthcare field, with a national shortage,* demand for qualified medical coders and billers is only expected to grow!
Student Life
Student Life
December 8, 2025
10 Successful Tips for Online Learning
Learning online is a great alternative to a traditional classroom, to help you succeed, here are ten proven strategies to help your experience.
Student Life
May 2, 2023
Supporting a Healthy Mind & Body
Taking care of your mind and body are important skills, and like all skills, it must be developed and practice. These resources can help you get on the right track.
Student Life
November 1st, 2022
High School Bullying Guide
Bullying looks different at different ages and also takes on many different forms. Some bullying involves physical violence; this is very common among young children.
Student Life
November 2nd, 2022
The School Counselor's Role in Bully Prevention
By high school, almost everyone has had some experience with bullying either as a victim, a bystander, or as a bully.
High School
High School
August 31, 2022
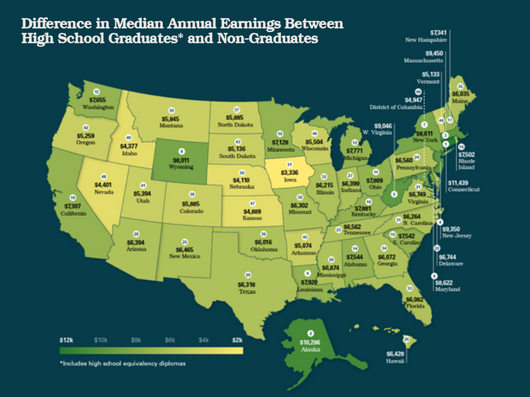
How Much More Do High School Grads Earn Than Non-Grads
Is getting your high school diploma worth it? Most likely! People who have a high school diploma statistically make more than those who never graduate. Review the earnings gaps by state now!
High School
August 15, 2022
Best High School in Each State
A great high school can be a huge factor in your decision on where to move. U.S. Career Institute has put together a guide on the best high school in every state! See if your school makes the list now!
High School
August 25, 2022
USCI Online High School Diploma
There are a variety of ways that you can receive your high school diploma. Beyond going to an in-person school, there are also online options available. Online high school is a great option for both adult and teens!
High School
August 18, 2022
Online High School Program for Adults
Returning to high school as an adult can be challenging, it will take discipline, motivation, and courage, but it is possible! Choosing a program that will work for your lifestyle is essential to ensure your success!
USCI News
USCI News
June 6, 2025
USCI Online High School Program Awarded MSA-CESS Accreditation
U.S. Career Institute is proud to announce that our Online High School program has awarded MSA-CESS Accreditation. Learn more here!
USCI News
July 26, 2022
USCI Launches New High School
U.S. Career Institute is proud to announce the launch of our new online high school! Whether you are an adult going back to school or a traditional student looking for alternative high schools, our program is perfect for you!
USCI News
November 16, 2022
U.S. Career Institute Launches Two Programs
U.S. Career Institute now has two new exciting programs! Explore the opportunities of your new exciting career as a phlebotomy technician or a HVACR technician. Learn more now.
USCI News
July 19, 2022
U.S. Career Institute Celebrates 40 Years of Education Excellence
Providing 40 years of education excellence, U.S. Career Institute is celebrating their 40th year anniversary. We are proud to have served the online learning community with flexible, quality distance education for the last 40 years.
Career Advice
Career Advice
November 14, 2025
Top 5 Factors Affecting Earning Potential
There are a number of factors that may be influencing your earning potential! Learn the top 5 factors and what you can do about them!
Career Advice
May 1, 2025
22 Healthcare Careers Requiring an Associate Degree or Less
Interested in a career in healthcare but intimidated by the schooling requirements? USCI has put together a list of healthcare careers you can do with an associate degree or less!
Career Advice
March 12, 2025
Celebrating Women Leaders in America's Top Industries
Women have played an improtant part in many industries throughout the history of the USA. Celebrate Women's Hisotry month by learning more about some of these amazing women!
Career Advice
November 13, 2023
Benefits of a Vocational Education
A vocational education can help you get a career without having to spend a ton of money and time on a college education. Vocational education has many benefits beyond that, learn more now!
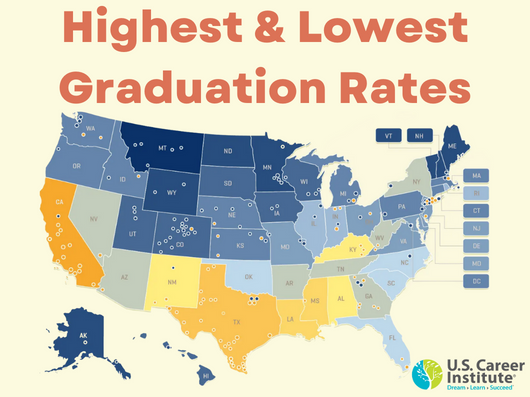
Academics
Academics
August 19, 2022
Highest and Lowest Graduation Rates
Finishing high school is a major achievement! Although High School graduation rates have been on the rise over the past decade, there are still some states and counties that have low graduation rates.
Academics
August 5, 2022
Online Learning at USCI
Continuing your education can have a positive impact on your life and career. Online education at USCI allows you to continue your education while studying at your own pace, on your own time, and wherever you want.
Academics
May 28, 2022
Future of Online Learning
Thanks to advances in new technology and internet access education is changing everyday. What does the future of online education look like? Learn more about where online education is going.
Academics
May 19, 2022
Equipped for a Career
USCI offers a variety of certificate and associate degree programs that can help you prepare for a career. USCI can help you be equipped for a career of your choice, read more now to learn how.