What Are Medical Claims and How Are They Processed?
By: Jenn Hall | February 2026
A medical claim is a formal invoice or bill generated by healthcare providers after a patient visit to request payment from the patient’s insurance provider for services rendered. The medical claim will include details of the visit and their respective billing codes, including diagnoses, procedures, and treatments. Any amount that is not covered by the insurance plan will be billed to the patient.
Medical claim accuracy is essential to ensure they are processed quickly and correctly. An error in the medical claim can cause unnecessary back and forth between the patient, insurer, and medical practice, leading to payment delays or even claim denial. This may cause financial strain on both the healthcare provider and patient, depending on the outcome.
How is a medical claim created and processed?
The journey of a medical claim begins before a patient schedules their appointment. Typically, healthcare providers will verify a patient’s insurance coverage, including whether the chosen doctor or practice is within network and whether the appointment type, procedure, or other treatment needs are covered by the insurance plan.
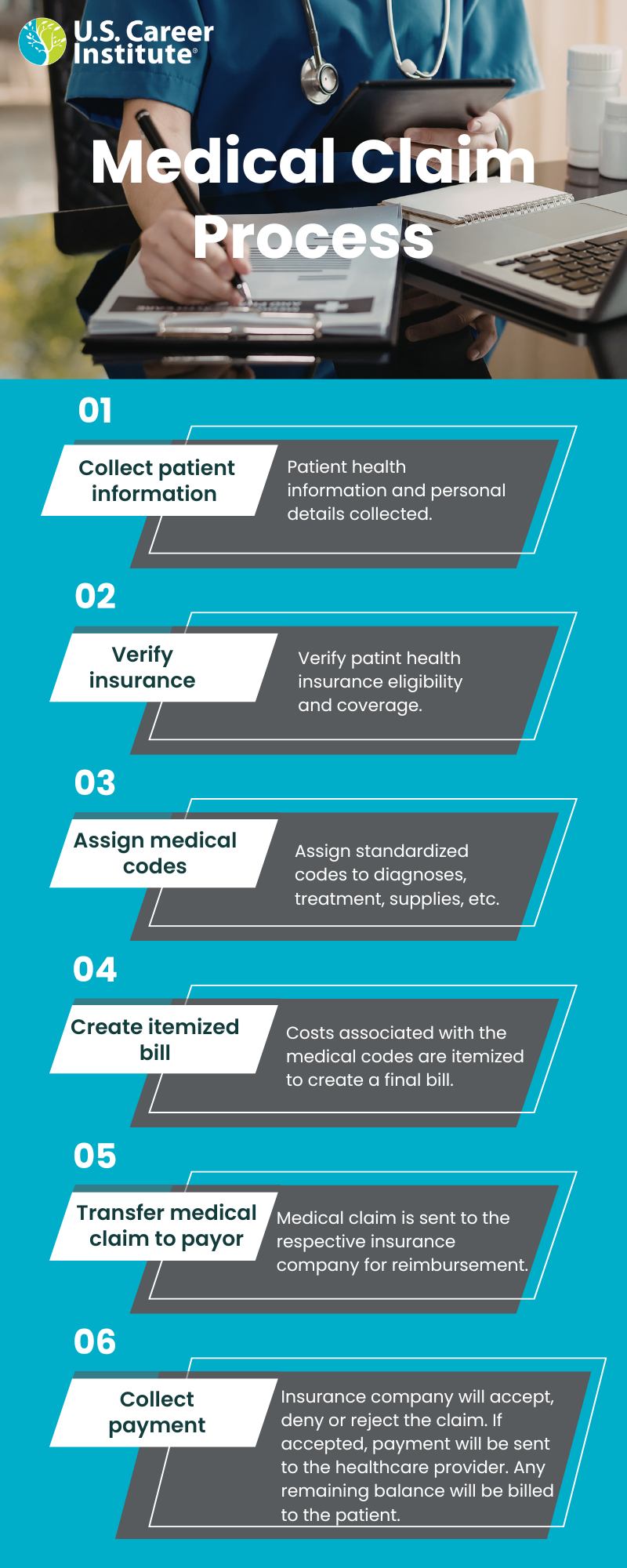
When creating and processing a claim the following steps must be followed:
- Collect patient information: Prior to the appointment, the patient's health information and personal details are collected. Healthcare teams typically use practice management (PM) software, electronic medical records (EMR), or a healthcare customer relationship management (CRM) solution to manage patient data, including insurance information. Patient data may be collected over the phone, in person, or through an online system.
- Verify insurance: Once the insurance information is gathered, typically a medical coding and billing specialist will verify the insurance information s to ensure that the visit is covered under the patient's insurance policy. This also helps determine what the patient's copay is and if the patient needs pre-approval for any treatment or intervention. Copays are important for medical providers as it adds to their cash flow while they wait for payer reimbursement.
- Assign medical codes: After the patient receives care from the healthcare provider, the visit notes are sent to the medical coder, who transcribes the documentation into standardized medical codes. These codes are used to describe what medical procedures, diagnoses, prescriptions, and supplies were administered during the visit.
- Create itemized bill: After the medical coding is completed, the costs associated with each medical code are itemized on the medical claim, creating the final bill.
- Transfer medical claim to payer: Medical claims are typically transferred to the payer (i.e., insurance company) electronically. The frequency for sending medical claims will depend on the policies and procedures of the individual healthcare facility. For example, some healthcare providers will send medical claims daily, while others may opt to send them in bulk weekly or even monthly.
- Collect payment: Once the payor receives the medical claim, they will assess the claim in relation to the patient’s benefits. They will then determine whether to accept, deny, or reject the claim.
If the claim is accepted, the payor will reimburse the healthcare provider in accordance with the patient’s benefit plan. Reimbursement is not always 100% covered by the payor. For some services or treatments, the payor may reimburse for a portion of the total cost, leaving the remaining balance for the patient to cover. For example, if an insurance plan covers 80% of a particular procedure, then the remaining 20% will be covered by the patient until they reach their out-of-pocket maximum.
If a medical claim is rejected or denied, additional steps must be taken by the healthcare provider or patient. Rejections are often easily resolved by addressing any errors and resubmitting the medical claim. Denials are harder to address, however. Medical claims may be denied for a variety of reasons, including lack of pre-authorization or insufficient patient coverage. Regardless of the reason, the patient can file an appeal to their insurance provider. This process can be lengthy, so payment will be delayed.
After the insurance payor reimburses the healthcare provider for their portion of the fees, the any remaining balance will be billed to the patient.
Get involved: Medical claims are an essential part of the healthcare revenue cycle. They ensure that healthcare providers are paid for the care they provide to patients in a timely manner. Medical coding and billing specialists are at the forefront of creating and processing these medical claims, making them an important member of the healthcare team.
To learn more about becoming a medical coding and billing specialist, check out the following resources:
- Online medical coding and billing certificate program (can be completed in 5 – 12 months, part time)
- Online medical coding certificate program (can be completed in 4-11 months, part time)
- Online medical billing certificate program (can be completed in 4-7 months, part time)
- Career Outlook: Medical coding and billing (blog)
- 6 Reasons to become a medical coding and billing specialist (blog)
